The Praxis Planner
your personal journal for us to work together
Your mental health journey is unique, and The Praxis Planner is your personalized space to explore it. Through guided reflections, exercises, and real-time feedback, this journal fosters collaboration between you and your care team. Whether tracking what’s working or identifying areas for adjustment, The Praxis Planner helps us tailor your care to truly fit your needs. Let’s work together to transform insight into action, and action into lasting change.

Our Journal
The Enduring Power of Pen and Paper: How Analog Practices Support Mental Health
This article highlights the enduring significance of analog practices—writing, doodling, drawing, and journaling—as essential tools for mental well-being, cognitive enhancement, and personal growth. Grounded in both historical tradition and modern neuroscience, these activities stimulate complex motor and cognitive processes that digital interactions often neglect. Research demonstrates that handwriting improves memory retention, promotes emotional regulation, and fosters mindfulness by slowing mental processes and grounding individuals in the present moment. Additionally, expressive writing and creative drawing serve as therapeutic outlets for processing emotions, reducing anxiety and depression, and supporting overall mental health. As part of a holistic approach to care, Praxis Mental Health encourages integrating these analog practices into both therapeutic work and personal wellness rituals, providing a much-needed counterbalance to the overstimulation of modern digital life.

The Praxis Standard: Elevating Mental Health Care Through Thoughtful, Comprehensive Treatment
This article explores the Praxis Signature Framework, our model of elevated mental health care that integrates advanced psychiatric expertise with depth-oriented psychotherapy to deliver highly personalized, evidence-based treatment. Moving beyond routine medication management, we emphasize continuous reassessment, patient education, and shared decision-making to foster meaningful therapeutic progress. This journal entry highlights, through a case reflection, the importance of evaluating treatment effectiveness and discussing milestones in care. This entry underscores the need for clinicians to remain actively engaged in their patients’ mental health journeys. The Praxis Mental Health approach combines individualized, data-informed treatment plans with clear patient education and responsive support from the multidisciplinary team, including registered nurses. Our model exemplifies a higher standard of psychiatric and therapeutic care, aiming to empower patients and improve long-term outcomes through collaboration, curiosity, and compassionate care.

Being of Service to Mothers Means Listening First
This article explores the critical role of deep, attuned listening as the foundation for effective maternal mental health care. In a healthcare landscape that often prioritizes efficiency and symptom management, the act of slowing down to truly hear a mother’s story becomes a radical and transformative intervention. Drawing from psychodynamic principles, the author illustrates how emotions frequently labeled as pathological—such as anxiety, anger, or overwhelm—often carry deeper relational and existential meaning within the context of new motherhood. Through clinical reflection and personal experience, the piece underscores the importance of honoring the full emotional landscape of motherhood, including grief, joy, ambivalence, and vulnerability. By creating therapeutic spaces that foster emotional honesty and connection, providers can move beyond prescriptive checklists to develop more accurate, compassionate, and effective treatment plans. The author advocates for a model of care rooted in relational presence, where listening is not a passive act but an essential service that empowers mothers to feel seen, validated, and capable in their transition to motherhood.

Scholarship as a Form of Care: How Curiosity Shaped My Career
This narrative explores the author’s professional journey from licensed Marriage and Family Therapist to psychiatric nurse practitioner, illustrating how a foundation of curiosity and scholarship shaped a career devoted to integrative mental health care. Recognizing the limitations of a single-modality approach, the author pursued advanced training to bridge the gap between psychotherapy and psychiatry, blending relational insight with medical expertise. This career path exemplifies how ongoing scholarship—through the continuous study of neurobiology, pharmacology, and psychological research—can directly enhance patient care. Rather than viewing academic inquiry as separate from clinical work, the author describes how curiosity fuels a practice rooted in collaboration, education, and evidence-informed treatment. This model positions scholarship not as an academic exercise, but as an essential form of care that empowers patients through both understanding and meaningful therapeutic change.

Why Therapeutic Rapport Matters
This article highlights the often-overlooked yet critical role of the therapeutic relationship in psychiatric care, particularly in the context of medication management. While pharmacological efficacy is essential, research consistently demonstrates that the quality of the patient-provider relationship significantly influences treatment outcomes, adherence, and patient satisfaction. Studies show that perceived warmth, trust, and emotional support from providers enhance both engagement and clinical success, regardless of the medication prescribed. Integrating psychotherapy skills such as empathic listening, motivational interviewing, and reflective dialogue into psychiatric practice strengthens therapeutic rapport and supports meaningful behavior change. Drawing from both research evidence and clinical experience, the author advocates for a model of care in which medication management and relational presence work synergistically to improve mental health outcomes. In this approach, the provider’s ability to listen deeply and foster trust becomes as powerful a tool as the medications themselves.

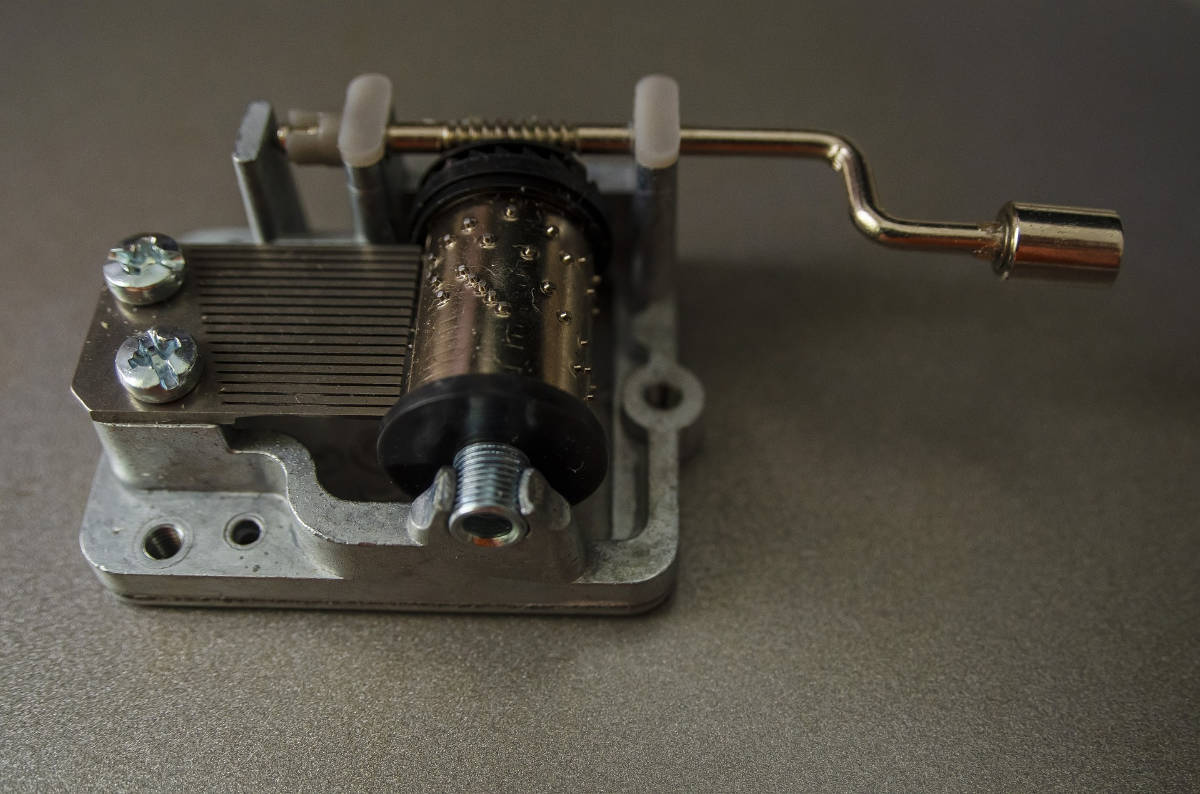
Meaning of Praxis
This article explores the integration of psychodynamic psychotherapy principles with actionable strategies to foster meaningful and lasting change in mental health care. Using the metaphor of a wind-up music box, the author illustrates how unconscious experiences, early relational patterns, and unexamined memories shape emotional responses and behaviors. While gaining insight into these hidden influences is foundational, the author argues that true transformation requires applying that insight through deliberate action—whether behavioral changes, therapeutic interventions, medication, or lifestyle modifications. This combination of reflection and action allows individuals to adjust long-standing emotional patterns and improve psychological well-being. The Praxis model embodies this philosophy, offering a comprehensive approach to mental health that honors both deep self-understanding and the concrete steps necessary to create lasting, positive change.